Administering Assessments: The Pragmatics of Measurement-Based Care (MBC)

Description
Once a clinician or a system of care has made the commitment to implement MBC, we soon find that the devil is in the details. Like most initiatives, the pragmatics involved in MBC, particularly administering the assessment to patients and collecting responses, is critical to its success. The challenge is to collect useful and actionable information without burdening patients, clinicians or administrators. In this blog, I will discuss the major challenges to administering assessment to patients and touch upon the CarePaths solution. As with any systemic initiative, there are tradeoffs to consider, depending on the context and priorities.
How to Introduce MBC to Patients
The success of MBC depends entirely on the patients’ agreement to complete the instruments faithfully and truthfully. If patients believe that completing the instruments will improve the process and outcome of psychotherapy, they are more likely to spend the necessary time and effort. We suggest making some variation of the following points to the patient: “Your progress in therapy and achievement of your goals is the primary focus of your therapy. It makes intuitive sense, and there is overwhelming research evidence as well, that information about your progress and your perceptions of the therapeutic process can significantly improve your outcomes. The few minutes it takes to complete the instruments will greatly increase the quality of your care.”
How Often to Administer Assessments
As a general rule, the more information the better. But of course, frequent measurement can be a burden for patients and difficult for therapists to process. Often MBC assessments are done on a session basis —symptoms and functioning just before the session commences and perceptions of the process at the end of the session. This is convenient because the patient is present (either face-to-face or via video), but there are several disadvantages to this approach. First, sessions may occur irregularly, and if it has been several weeks since the previous session, the therapist will have little information about patient functioning during this period. Second, completing measures in proximity to seeing the therapist may create demand expectations for the patient—some patients will not want to disappoint their therapist, who they will soon see or will have just seen, by indicating that they are not progressing or therapy is not going well. Third, there is insufficient time for the therapist to process the information and plan for or alter therapy. We recommend that the progress and process of therapy be measured every week, regardless of the frequency of sessions, and that they not be administered immediately prior to or after a session.
How to Administer the Assessments
Given that we are choosing not to synchronize measurement with therapy sessions, going through assessments verbally with the patient or having them fill out a paper form are simply not practical. Since most people are already accustomed to responding to various inquiries online, we recommend prompting patients with texts or emails, with links to electronic forms of the assessments. That way patients can then respond at their convenience. We also recommend breaking up the assessments into parts, so that the time for any one assessment is less than 3 minutes or so. If assessments are not completed, reminders can be sent, with personal messages from the therapist about the importance of the assessment. If patients are consistently notcompleting assessments, the therapist should discuss this with the patient, in a collaborative manner.
We should note that some patients find the assessments disagreeable and decline the invitation to participate. After discussing MBC, the therapist and the patient may decide to forego it– MBC provides information but it is only useful if both the therapist and patient embrace the practice.
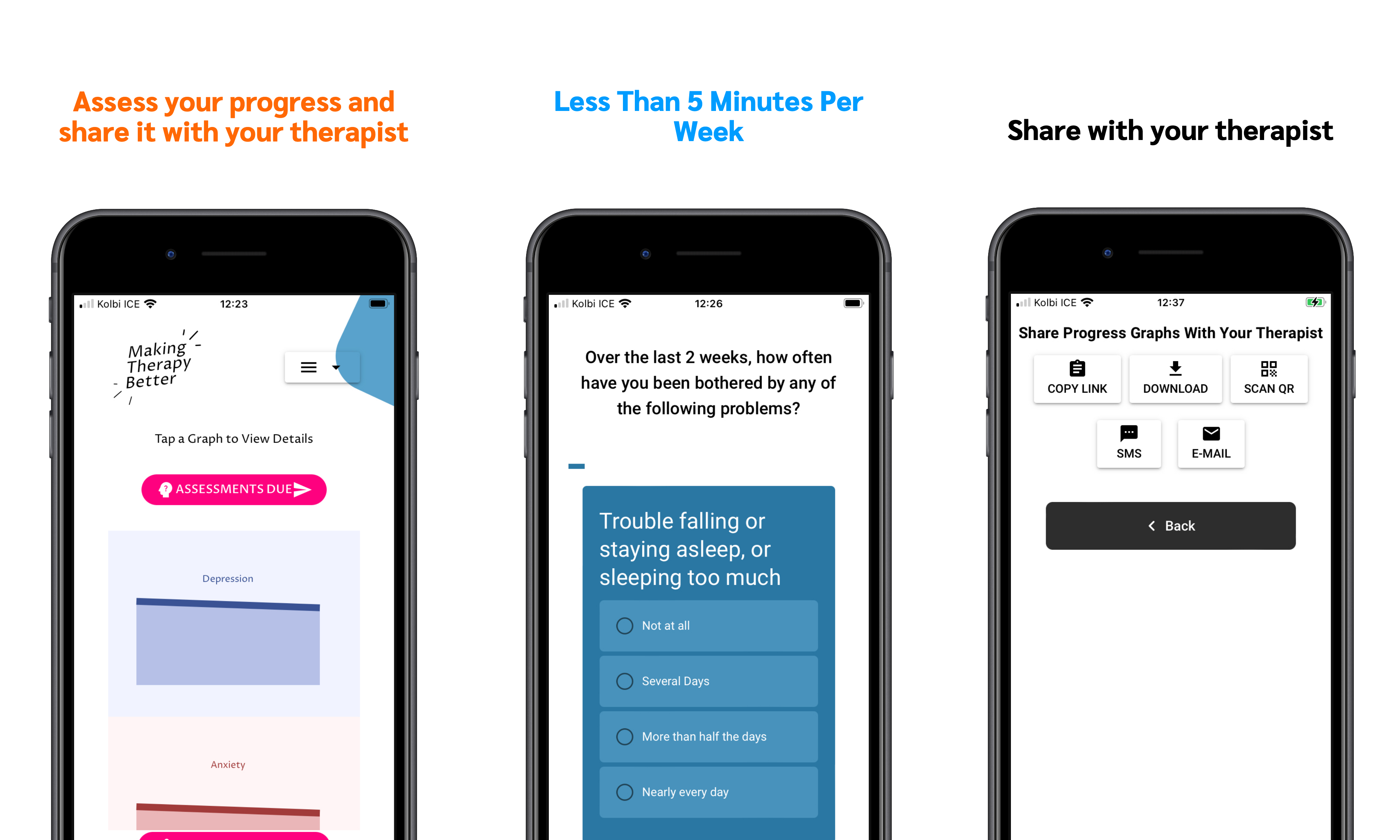
The CarePaths Solution
With the exception of talking to your patients about the reasons to complete regular assessments, the CarePaths MBC protocol addresses all the challenges of administering MBC assessments. The carefully chosen measures (see our last blog [link]) are sent to the patient every week. The patient is assigned two notifications at a time so completing them only takes a few minutes, with one set of two assessments on Monday, Wednesday and Friday. The patient receives a notification via text message and/or email with a link to complete the assessment in the CarePaths Connect app, or in their patient portal in a browser. Their results are automatically scored and the data added to a chart that is visible by both the therapist and the patient.
Although the process is automated, it’s important for the clinician to remember that their part in the MBC process really begins after the assessments have been administered. The information collected is useful only if the therapist discusses it with the patient and uses it to guide therapy, creating a collaborative process. In my next post I’ll be discussing these last two critical steps in the practice of MBC.